Abstract
INTRODUCTION: Heparin-induced thrombocytopenia (HIT) is a pro-thrombotic process from heparin administration followed by anti-heparin antibody formation and antibody-mediated platelet (PLT) activation leading to thrombin generation. We report the 1st case of HIT refractory to multiple anticoagulants, steroids and intravenous immunoglobulin (IVIg), which responded to Rituximab.
CASE REPORT:
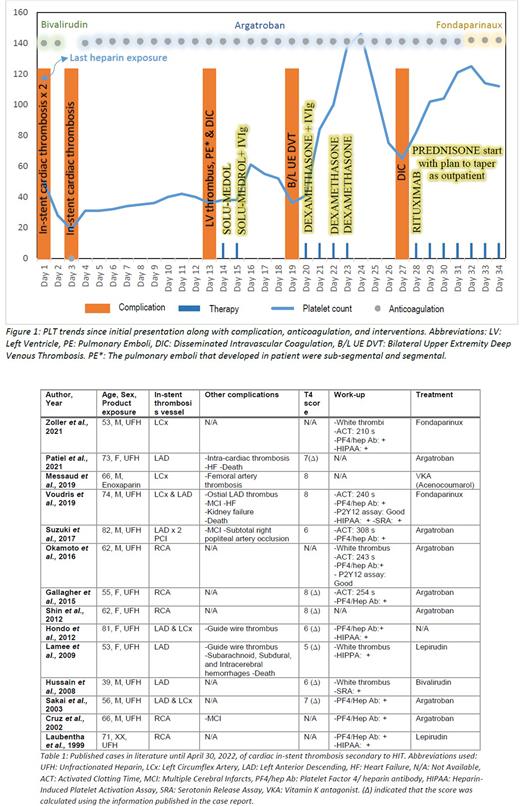
A 57-year-old male presented with recurrent chest pain one day after discharge for ST-elevation myocardial infarction (STEMI) requiring stent placement. Repeat EKG showed new STEMI and he had a decreased PLT count of 50,000/mm3 from 224,000/mm3 the prior day. The recently placed stent was ballooned during Percutaneous Coronary Intervention (PCI). Within hours, a 2nd PCI was required for repeat stent occlusion. HIT was suspected because of the recurrent in-stent thrombosis and thrombocytopenia after heparin re-exposure. The 4T score was 7 with PLT fall > 50% with nadir > 20,000/mm3 (+2), onset of fall between day 5-10 of heparin exposure (+2), development of in-stent thrombosis (+2), with other possible causes of thrombocytopenia (+1). His PLT factor 4 antibody was elevated. Bivalirudin was started and last heparin exposure was on day 1 (figure 1). On day 3, the patient had a recurrent STEMI, required 3rd PCI while on Bivalirudin. On day 5, Bivalirudin was switched to Argatroban, given no improvement and better institution protocol for monitoring. While on Argatroban, the course was complicated by a new left ventricular thrombus, multiple pulmonary embolisms, and disseminated intravascular coagulation (DIC). Given recurrent thromboses without heparin re-exposure, the patient received methylprednisolone 250 mg every 6 hours on days 14-15 and IVIg 1g/kg on day 15 with transient improvement in PLT to 61,000/mm3 on day 16. On day 19, he developed new bilateral upper extremity deep vein thromboses, prompting a 2nd course of IVIg 1g/kg daily on days 20-21 and dexamethasone 40mg IV daily on day 20-23. His PLT transiently responded, but he again developed DIC on day 27. He was started on prednisone 1mg/kg daily with a 4-6 week taper. On day 28, he was given Rituximab 375 mg/m2 with a weekly plan for four weeks. His PLTs improved to 112,000/mm3, and he was discharged home on Fondaparinaux. His PLTs recovered to baseline of 231,000/mm3 by day 53 and PF4/hep Ab became undetectable by day 141 without complications.
DISCUSSION: This is the first reported case of refractory HIT complicated by cardiac in-stent thrombosis resistant to multiple anticoagulants, steroids, and IVIg that ultimately responded to Rituximab. HIT induced cardiac in-stent stenosis is a crucial diagnosis while evaluating in-stent thrombosis as anticoagulation bolus is needed during PCI (Table 1). There is minimal data to date on refractory HIT and the role of immunosuppression. In 2013, Schell et al. reported the use of Rituximab in refractory HIT, however the efficacy of Rituximab could not be assessed due the development of gangrenous limb affecting PLT count. In our case, the patient had recurrent thromboses and thrombocytopenia while on a direct thrombin inhibitor that clearly responded to immunosuppression consistent with autoimmune HIT after exposure to heparin.
CONCLUSION: Given the rarity of HIT, there are no management guidelines for the treatment of refractory disease, and such cases remain a challenging clinical scenario. More work is needed to understand if all cases of refractory HIT have an autoimmune component and the role of Rituximab.
Disclosures
Poston:TeraImmune: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal